Plastic Predators: Hospital Superbugs Now Devouring Life-Saving Medical Devices
It's a vicious cycle," notes Dr. Robert Williams, an infection control specialist. "The bacteria damage the plastic, which creates more places for bacteria to hide, which leads to more damage. Meanwhile, our standard cleaning protocols may not be addressing these newly created bacterial reservoirs

In the ongoing battle against hospital-acquired infections, healthcare professionals face a startling new challenge: antibiotic-resistant bacteria eating away at the medical devices designed to help patients heal. This unexpected discovery has profound implications for infection control practices and patient safety in healthcare settings worldwide.
The Hidden Threat in Hospital Rooms
When Emma Thompson entered the hospital for a routine procedure, she never expected to leave with a life-threatening infection. Two weeks after her discharge, she was rushed back to the emergency room with symptoms of a severe bacterial infection. The culprit? A superbug that had colonised her IV catheter, hiding in microscopic cracks in the plastic that standard sterilisation procedures failed to reach.
While Emma's case is hypothetical, it represents a growing concern in healthcare facilities globally. Hospital-acquired infections (HAIs) affect millions of patients annually, and the rise of antibiotic-resistant "superbugs" has complicated treatment options. Researchers have identified an alarming new factor: certain superbugs can break down the medical plastics they colonise, creating perfect hiding spots that enhance their survival and spread.
What Are Hospital Superbugs?
Hospital superbugs have developed resistance to most conventional antibiotics, making infections extremely difficult to treat. These microbial menaces have evolved through natural selection, as we've used antibiotics extensively over decades, bacteria that randomly developed resistance mechanisms survived and multiplied, while susceptible bacteria died off.
Common hospital superbugs include:
- Methicillin-resistant Staphylococcus aureus (MRSA): A leading cause of skin, wound, and bloodstream infections
- Pseudomonas aeruginosa: Often found in medical equipment and known for its adaptability
- Acinetobacter baumannii: Nicknamed "Iraqibacter" due to its prevalence in military hospitals during Middle Eastern conflicts
- Carbapenem-resistant Enterobacteriaceae (CRE): A family of bacteria highly resistant to our strongest antibiotics
These pathogens pose significant risks in healthcare settings because they spread easily, resist treatment, and can cause severe complications in vulnerable patients.
Medical Plastics: The Backbone of Modern Healthcare
Look around any hospital room, and you'll find plastics everywhere. From IV tubes and catheters to syringes, ventilator components, and protective equipment. Medical-grade plastics have revolutionised healthcare delivery, and their popularity stems from several key advantages:
- Cost-effectiveness: Allowing for affordable, single-use items that reduce cross-contamination
- Durability: Withstanding various physical stresses without breaking
- Versatility: Being moulded into countless specialised shapes and devices
- Sterility: Easy to produce in sterile conditions and maintain cleanliness

Medical devices made from plastics like polyvinyl chloride (PVC), polyethylene, polypropylene, and silicone were long thought to be relatively inert-stable materials that wouldn't interact significantly with the human body or its microscopic inhabitants. This presumed stability has been a cornerstone of medical device safety... until now.
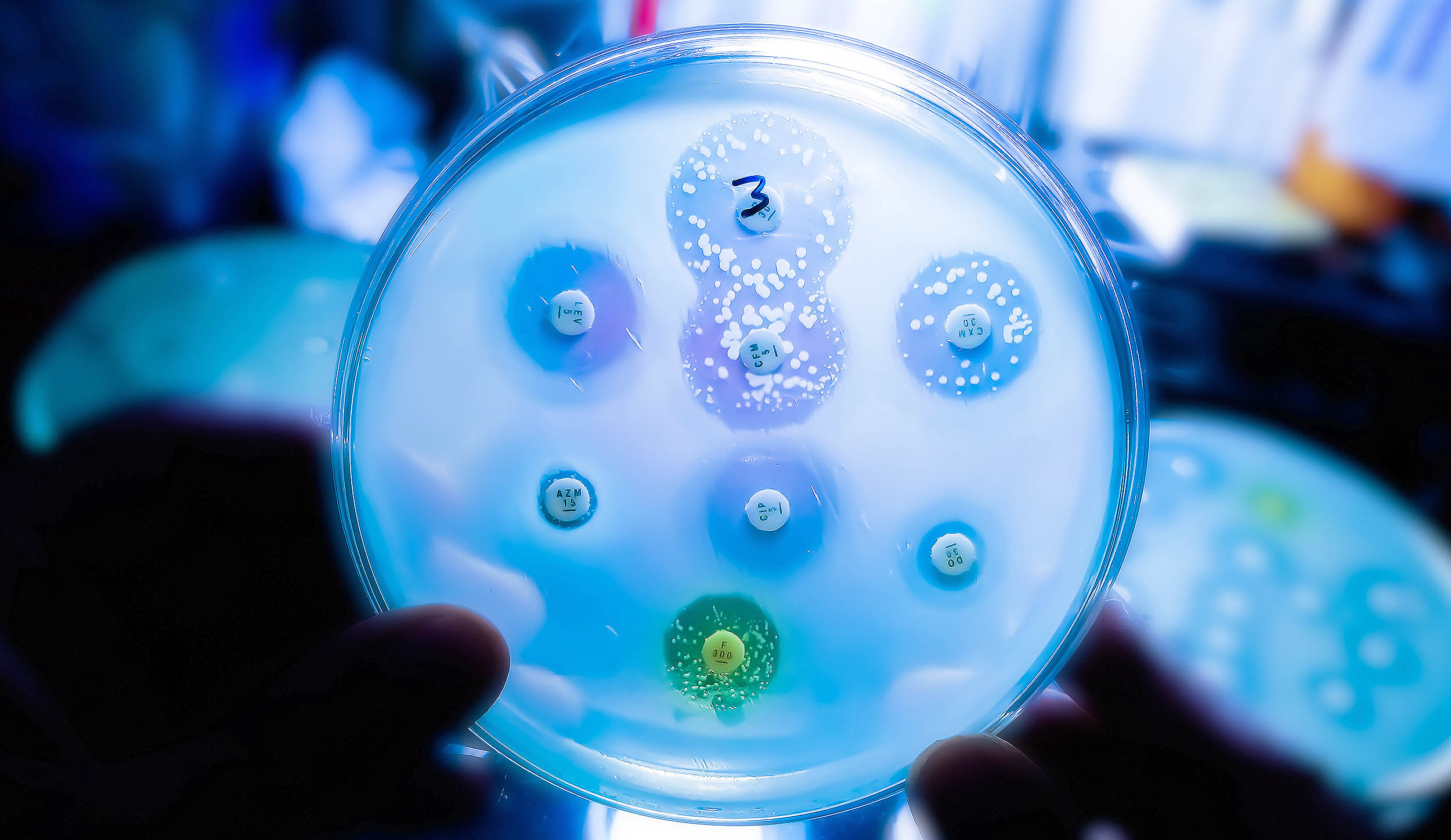
The Startling Discovery: Superbugs That Eat Plastic
Recent research has revealed something unsettling: certain antibiotic-resistant bacteria can metabolise and degrade medical plastics. These microorganisms have developed enzymatic pathways that allow them to break down plastic polymers, using them as a food source while simultaneously creating microscopic damage to the material.
Dr Sarah Chen, a microbiologist specialising in bacterial resistance mechanisms, explains:
"We've observed certain strains of Pseudomonas and Acinetobacter that can slowly degrade common medical plastics. They create tiny fissures and irregularities in surfaces that were designed to be smooth and impermeable. It's as though they're remodelling their environment to better suit their needs."
This degradation happens slowly but progressively. Under powerful electron microscopes, researchers can observe how formerly smooth plastic surfaces develop rough patches, cracks, and pits when exposed to these bacteria, particularly when those devices remain in place for extended periods.

How Plastic Degradation Creates the Perfect Storm for Infections
The implications of this discovery extend far beyond interesting microbiology. When bacteria degrade plastic medical devices, they create several dangerous conditions:
Microscopic Hiding Places
Imagine trying to clean a scratched cutting board compared to a smooth one. Just as food particles can hide in a cutting board, bacteria can shelter in the microscopic crevices they create in plastic devices. Standard cleaning and sterilisation protocols may not reach these protected microorganisms.
Biofilm Formation
These degraded areas provide ideal attachment points for bacterial biofilms—complex communities of microorganisms that secrete a protective matrix. Biofilms can be up to 1,000 times more resistant to antibiotics and disinfectants than free-floating bacteria.
Direct Access to the Body
With invasive devices like catheters and feeding tubes, degradation can create pathways for bacteria to access the bloodstream or other normally sterile areas.

Reduced Effectiveness of Medical Devices
As plastics degrade, the devices may function less effectively, potentially requiring more frequent replacements and additional procedures, each representing a new infection opportunity.
"It's a vicious cycle," notes Dr. Robert Williams, an infection control specialist. "The bacteria damage the plastic, which creates more places for bacteria to hide, which leads to more damage. Meanwhile, our standard cleaning protocols may not address these newly created bacterial reservoirs."
The Main Culprits: Which Superbugs are Plastic Eaters?
Not all bacteria can degrade plastics, but several hospital pathogens have demonstrated this ability:
Pseudomonas aeruginosa leads the pack with its remarkable adaptability. This opportunistic pathogen produces enzymes that can break down various compounds, including components of certain plastics. Its ability to form robust biofilm compounds the problem.
Acinetobacter baumannii, already notorious for surviving on dry surfaces for extended periods, has been shown to slowly degrade certain medical polymers, particularly those used in respiratory equipment.
Certain strains of Klebsiella pneumoniae and Enterococcus faecalis have also demonstrated plastic-degrading capabilities in laboratory settings, though typically to a lesser extent than Pseudomonas.
What makes these bacteria particularly concerning is their simultaneous resistance to multiple antibiotics, creating a perfect storm of persistence, adaptability, and treatment resistance.
The Real-World Impact: From Hospital Rooms to Recovery Outcomes
The Consequences of Plastic-Degrading Superbugs Extend Throughout the Healthcare System:
For Patients
Patients with long-term indwelling devices like central lines, urinary catheters, or feeding tubes face the highest risk. When bacteria colonise and degrade these devices, patients may experience:
- Persistent or recurring infections despite appropriate antibiotic therapy
- Longer hospital stays
- Additional surgical procedures to replace compromised devices
- Increased exposure to broad-spectrum antibiotics, which can disrupt beneficial microbiomes
For Healthcare Facilities
Hospitals and clinics face significant challenges:
- Higher rates of healthcare-associated infections affect quality metrics
- Increased costs associated with treating complications
- More frequent device replacements
- Need for enhanced sterilisation protocols
For Public Health
The broader implications include:
- Acceleration of antibiotic resistance as more antibiotics are used to treat device-associated infections
- Greater pressure on healthcare systems already strained by resistant infections
- Potential for outbreaks when plastic-degrading strains spread within facilities
Innovation at the Frontlines: Solutions Taking Shape
The medical community isn't standing idle in the face of this challenge. Several promising approaches are being developed:

New Materials Science
Researchers are developing new polymers designed specifically to resist bacterial degradation. Some incorporate antimicrobial properties directly into the plastic through surface modifications or embedded compounds that slowly release over time.
"We're exploring materials that can actively repel bacterial attachment," explains Dr. Jennifer Lopez, a biomedical engineer developing next-generation catheter materials. "By creating surfaces that prevent initial colonisation, we hope to break the cycle before it begins."
Enhanced Sterilisation Techniques
Recognising that traditional methods may not suffice, hospitals are implementing more rigorous protocols:
- Ultrasonic cleaning that reaches into microscopic crevices
- Advanced hydrogen peroxide vapour systems for room decontamination
- UV-C light treatments for surfaces and equipment
Shorter Device Dwelling Times
Medical practice is evolving to minimise the time that devices remain in place:
- Daily reassessment of the need for catheters and lines
- Stricter protocols for device removal when no longer essential
- Alternative treatment approaches that reduce reliance on indwelling devices
What Can Patients and Families Do?
While medical professionals lead the charge against plastic-degrading superbugs, patients and families play crucial roles in protection:
Ask Questions
Don't hesitate to inquire about:
- How long do devices like catheters need to remain in place
- What infection prevention measures are being taken
- When devices were last changed or inspected
Practice Good Hygiene
- Follow hand hygiene protocols when visiting hospitalised loved ones
- Avoid touching medical devices unnecessarily
- Report any signs of redness, swelling, or discharge around device insertion sites
Be Informed About Antibiotics
- Take antibiotics exactly as prescribed
- Never save antibiotics for later use
- Understand that not all infections require antibiotics
The Road Ahead: A Multidisciplinary Challenge
Addressing plastic-degrading superbugs requires collaboration across disciplines. Microbiologists, materials scientists, infection control specialists, and frontline clinicians must work together to develop comprehensive solutions.
"This isn't just a microbiology problem or an engineering problem—it's both," says Dr. Chen. "We need to understand the bacterial mechanisms while simultaneously developing materials and protocols that can withstand them."
Research funding is increasingly directed toward this intersection of infectious disease and materials science, recognising the potential impact on patient outcomes and healthcare costs.
Vigilance in a Changing Landscape
The discovery that hospital superbugs can degrade medical plastics represents both a challenge and an opportunity for healthcare. While we have new concerns about infection control, it drives innovation in materials, practices, and awareness.
The message is clear for healthcare providers: device maintenance, timely replacement, and enhanced sterilszation must become priorities. For patients, understanding these risks empowers more active participation in care decisions and infection prevention.
As we continue to study this phenomenon, one thing remains certain: the microscopic battle between bacteria and the materials we create continues to evolve. Our success in addressing this challenge will significantly impact the future of healthcare-associated infections and patient safety.